Swallowing disorders after thyroidectomy: a systematic review and meta-analysis
Swallowing disorders following thyroidectomy are common, even after surgery without confirmed complications. The purpose of the current systematic review is to investigate the prevalence of dysphagia at various time points after thyroidectomy, at the whole spectrum of it (total/partial, open/endoscopic, for benign/malignant disease).
Methods
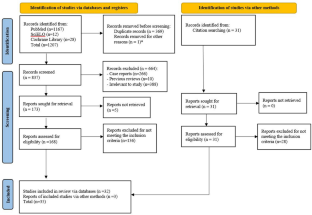
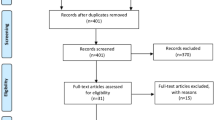
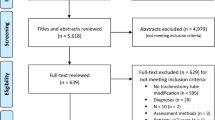
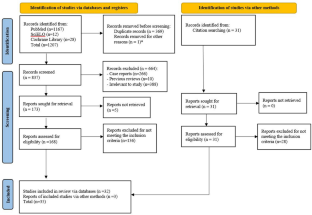
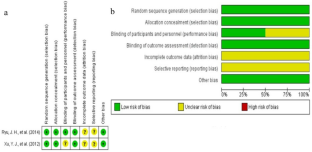
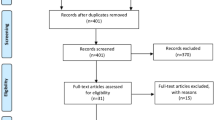
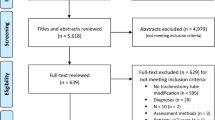
The literature available at PubMed, SciELO and Cochrane Library databases was reviewed, according to PRISMA guidelines, using the terms “dysphagia”, “swallowing disorder”, “deglutition disorder”, “thyroidectomy” and “thyroid surgery” in the appropriate combinations. A quantitative synthesis of the results followed.
Results
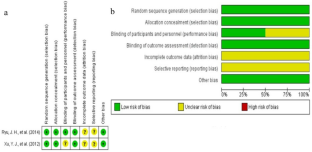
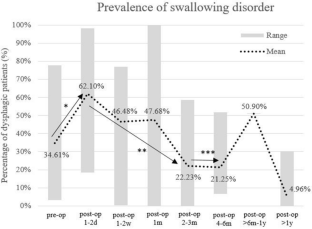
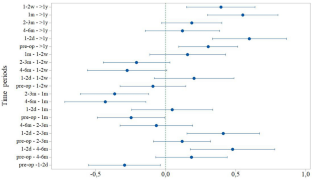
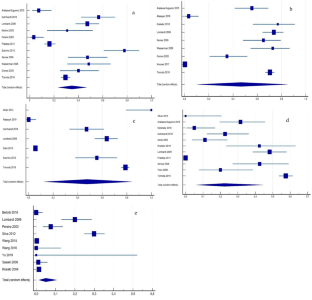
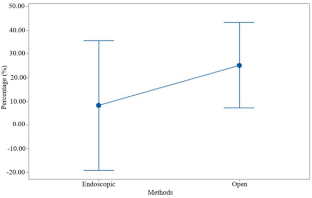
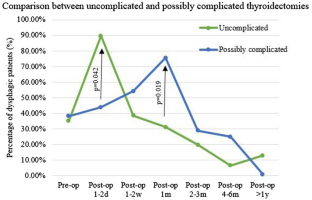
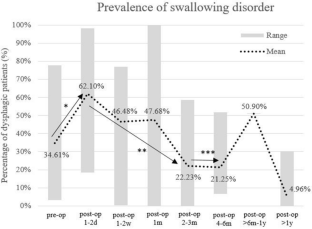
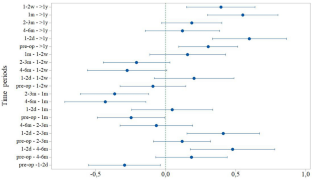
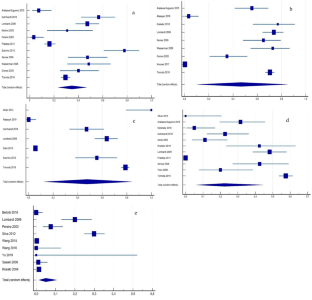
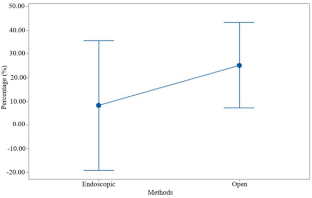
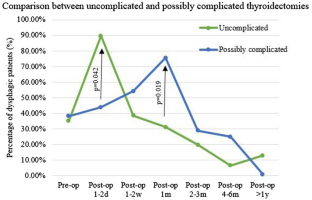
The systematic review of the literature resulted in 35 articles, which met the inclusion criteria and were analyzed regarding their type, sample, follow-up and results regarding post-thyroidectomy dysphagia in multiple follow-up times. A significant increase of swallowing impairment compared to baseline was recorded shortly after surgery. Dysphagia reverted to pre-operative levels 2–3 months later. Dysphagia continued to be reported in a significantly lower proportion of patients, even 1 year after surgery. No significant difference was noticed between open and endoscopic thyroid surgery at 2–3 months post-surgery.
Conclusions
The swallowing disorders reported after thyroidectomy should be expected, but are not always detectable through objective methods. This should not lead to underestimation of symptoms, since the patients’ quality of life is negatively affected by the symptomatology.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save
Springer+ Basic
€32.70 /Month
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Buy Now
Price includes VAT (France)
Instant access to the full article PDF.
Rent this article via DeepDyve

Similar content being viewed by others
Dysphagia following uncomplicated thyroidectomy: a systematic review
Article 14 August 2019
Changes in Swallowing Symptoms and Esophageal Motility After Thyroid Surgery: A Prospective Cohort Study
Article 11 October 2017
A Systematic Review of Tracheostomy Modifications and Swallowing in Adults
Article 06 May 2020
References
- Lombardi CP, Raffaelli M, De Crea C et al (2009) Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery 146(6):1174–1181. https://doi.org/10.1016/j.surg.2009.09.010ArticlePubMedGoogle Scholar
- Arakawa-Sugueno L, Ferraz AR, Morandi J et al (2015) Videoendoscopic evaluation of swallowing after thyroidectomy: 7 and 60 days. Dysphagia 30(5):496–505. https://doi.org/10.1007/s00455-015-9628-zArticlePubMedGoogle Scholar
- Galluzzi F, Garavello W (2019) Dysphagia following uncomplicated thyroidectomy: a systematic review. Eur Arch Otorhinolaryngol 276(10):2661–2671. https://doi.org/10.1007/s00405-019-05599-yArticlePubMedGoogle Scholar
- Printza A, Triaridis S (2021) Is the ability of the Eating Assessment Tool (EAT-10) to screen for aspiration in patients with dysphagia depending on the patients’ disease? Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-021-06661-4 (Epub ahead of print 2021/02/18) ArticlePubMedGoogle Scholar
- Park YM, Oh KH, Cho JG et al (2018) Changes in voice- and swallowing-related symptoms after thyroidectomy: one-year follow-up study. Ann Otol Rhinol Laryngol 127(3):171–177. https://doi.org/10.1177/0003489417751472ArticlePubMedGoogle Scholar
- Park KN, Mok JO, Chung CH et al (2015) Does postthyroidectomy syndrome really exist following thyroidectomy? Prospective comparative analysis of open vs. endoscopic thyroidectomy. Clin Exp Otorhinolaryngol 8(1):76–80. https://doi.org/10.3342/ceo.2015.8.1.76ArticlePubMedPubMed CentralGoogle Scholar
- Wasserman JM, Sundaram K, Alfonso AE et al (2008) Determination of the function of the internal branch of the superior laryngeal nerve after thyroidectomy. Head Neck 30(1):21–27. https://doi.org/10.1002/hed.20648ArticlePubMedGoogle Scholar
- Silva ICM, Netto IdP, Vartanian JG et al (2012) Prevalence of upper aerodigestive symptoms in patients who underwent thyroidectomy with and without the use of intraoperative laryngeal nerve monitoring. Thyroid 22(8):814–819. https://doi.org/10.1089/thy.2011.0118ArticlePubMedGoogle Scholar
- Gohrbandt AE, Aschoff A, Gohrbandt B et al (2016) Changes of laryngeal mobility and symptoms following thyroid surgery: 6-month follow-up. World J Surg 40(3):636–643. https://doi.org/10.1007/s00268-015-3323-yArticlePubMedGoogle Scholar
- Hillenbrand A, Cammerer G, Dankesreiter L et al (2018) Postoperative swallowing disorder after thyroid and parathyroid resection. Pragmat Obs Res 9:63–68. https://doi.org/10.2147/POR.S172059ArticlePubMedPubMed CentralGoogle Scholar
- Gumus T, Makay O, Eyigor S et al (2020) Objective analysis of swallowing and functional voice outcomes after thyroidectomy: a prospective cohort study. Asian J Surg 43(1):116–123. https://doi.org/10.1016/j.asjsur.2019.04.013ArticlePubMedGoogle Scholar
- Rommel N, Hamdy S (2016) Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol 13(1):49–59. https://doi.org/10.1038/nrgastro.2015.199ArticlePubMedGoogle Scholar
- Scerrino G, Tudisca C, Bonventre S et al (2017) Swallowing disorders after thyroidectomy: what we know and where we are. A systematic review. Int J Surg 41(Suppl 1):S94–S102. https://doi.org/10.1016/j.ijsu.2017.03.078ArticlePubMedGoogle Scholar
- Pradeep PV, Ragavan M, Ramakrishna BA et al (2011) Surgery in Hashimoto’s thyroiditis: indications, complications, and associated cancers. J Postgrad Med 57(2):120–122. https://doi.org/10.4103/0022-3859.81867ArticleCASPubMedGoogle Scholar
- Krekeler BN, Wendt E, Macdonald C et al (2018) Patient-reported dysphagia after thyroidectomy: a qualitative study. JAMA Otolaryngol Head Neck Surg 144(4):342–348. https://doi.org/10.1001/jamaoto.2017.3378ArticlePubMedPubMed CentralGoogle Scholar
- Tomoda C, Sugino K, Tanaka T et al (2018) Globus symptoms in patients undergoing thyroidectomy: relationships with psychogenic factors, thyroid disease, and surgical procedure. Thyroid 28(1):104–109. https://doi.org/10.1089/thy.2017.0524ArticlePubMedGoogle Scholar
- Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097ArticlePubMedPubMed CentralGoogle Scholar
- Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71ArticlePubMedPubMed CentralGoogle Scholar
- Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.xArticlePubMedGoogle Scholar
- Higgins JPT AD, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS (eds), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. www.training.cochrane.org/handbook. Accessed 1 Nov 2020
- Alkan Z, Yigit O, Adatepe T et al (2014) Effect of anti-adhesive barrier use on laryngotracheal movement after total thyroidectomy: an electrophysiological study. Indian J Otolaryngol Head Neck Surg 66(Suppl 1):71–77. https://doi.org/10.1007/s12070-011-0319-2ArticlePubMedGoogle Scholar
- Scerrino G, Inviati A, Di Giovanni S et al (2013) Esophageal motility changes after thyroidectomy; possible associations with postoperative voice and swallowing disorders: preliminary results. Otolaryngol Head Neck Surg 148(6):926–932. https://doi.org/10.1177/0194599813482299ArticlePubMedGoogle Scholar
- Sorensen JR (2018) The impact of surgery on quality of life, esophageal motility, and tracheal anatomy and airflow in patients with benign nodular goiter. Dan Med J 65(4):B5472 PubMedGoogle Scholar
- Araujo LF, Lopes LW, Silva POC et al (2017) Sensory symptoms in patients undergoing thyroidectomy. Codas 29(3):e20150294. https://doi.org/10.1590/2317-1782/20172016294ArticlePubMedGoogle Scholar
- Greenblatt DY, Sippel R, Leverson G et al (2009) Thyroid resection improves perception of swallowing function in patients with thyroid disease. World J Surg 33(2):255–260. https://doi.org/10.1007/s00268-008-9837-9ArticlePubMedPubMed CentralGoogle Scholar
- Sabaretnam M, Mishra A, Chand G et al (2012) Assessment of swallowing function impairment in patients with benign goiters and impact of thyroidectomy: a case control study. World J Surg 36(6):1293–1299. https://doi.org/10.1007/s00268-012-1562-8ArticlePubMedGoogle Scholar
- Burns P, Timon C (2007) Thyroid pathology and the globus symptom: are they related? A two year prospective trial. J Laryngol Otol 121(3):242–245. https://doi.org/10.1017/S0022215106002465ArticleCASPubMedGoogle Scholar
- Maung KH, Hayworth D, Nix PA et al (2005) Thyroidectomy does not cause globus pattern symptoms. J Laryngol Otol 119(12):973–975. https://doi.org/10.1258/002221505775010760ArticleCASPubMedGoogle Scholar
- Ben Nun A, Soudack M, Best LA (2006) Retrosternal thyroid goiter: 15 years experience. Isr Med Assoc J 8(2):106–109 PubMedGoogle Scholar
- Wang C, Sun P, Li J et al (2016) Strategies of laparoscopic thyroidectomy for treatment of substernal goiter via areola approach. Surg Endosc 30(11):4721–4730. https://doi.org/10.1007/s00464-016-4814-0ArticlePubMedGoogle Scholar
- Pereira JA, Girvent M, Sancho JJ et al (2003) Prevalence of long-term upper aerodigestive symptoms after uncomplicated bilateral thyroidectomy. Surgery 133(3):318–322. https://doi.org/10.1067/msy.2003.58ArticlePubMedGoogle Scholar
- Cho JG, Byeon HK, Oh KH et al (2020) Objective assessment of postoperative swallowing difficulty through ultrasound in patients undergoing thyroidectomy. Dysphagia 35(2):253–260. https://doi.org/10.1007/s00455-019-10020-1ArticlePubMedGoogle Scholar
- Almeida JP, Vartanian JG, Kowalski LP (2009) Clinical predictors of quality of life in patients with initial differentiated thyroid cancers. Arch Otolaryngol Head Neck Surg 135(4):342–346. https://doi.org/10.1001/archoto.2009.16ArticlePubMedGoogle Scholar
- Gal TJ, Streeter M, Burris J et al (2013) Quality of life impact of external beam radiotherapy for advanced thyroid carcinoma. Thyroid 23(1):64–69. https://doi.org/10.1089/thy.2012.0083ArticlePubMedGoogle Scholar
- Sahli Z, Canner JK, Najjar O et al (2019) Association between age and patient-reported changes in voice and swallowing after thyroidectomy. Laryngoscope 129(2):519–524. https://doi.org/10.1002/lary.27297ArticlePubMedGoogle Scholar
- Ikeda Y, Takami H, Sasaki Y et al (2002) Comparative study of thyroidectomies. Surg Endosc Other Interv Tech 16(12):1741–1745. https://doi.org/10.1007/s00464-002-8830-xArticleCASGoogle Scholar
- Atasayar S, Guler Demir S (2019) Determination of the problems experienced by patients post-thyroidectomy. Clin Nurs Res 28(5):615–635. https://doi.org/10.1177/1054773817729074ArticlePubMedGoogle Scholar
- Martins N, Novalo-Goto ES, Diz-Leme ICM et al (2020) Patient perception of swallowing after thyroidectomy in the absence of laryngeal nerve injury. ORL J Otorhinolaryngol Relat Spec 82(5):274–284. https://doi.org/10.1159/000508683ArticlePubMedGoogle Scholar
- Ryu JH, Yom CK, Park DJ et al (2014) Prospective randomized controlled trial on the use of flexible reinforced laryngeal mask airway (LMA) during total thyroidectomy: effects on postoperative laryngopharyngeal symptoms. World J Surg 38(2):378–384. https://doi.org/10.1007/s00268-013-2269-1ArticlePubMedGoogle Scholar
- Chung EJ, Park MW, Cho JG et al (2015) A prospective 1-year comparative study of endoscopic thyroidectomy via a retroauricular approach versus conventional open thyroidectomy at a single institution. Ann Surg Oncol 22(9):3014–3021. https://doi.org/10.1245/s10434-014-4361-7ArticlePubMedGoogle Scholar
- Lee DY, Lim S, Kang SH et al (2016) A prospective 1-year comparative study of transaxillary total thyroidectomy regarding functional outcomes: is it really promising? Surg Endosc 30(4):1599–1606. https://doi.org/10.1007/s00464-015-4386-4ArticlePubMedGoogle Scholar
- Jian CX, Wu LM, Zheng ZF et al (2020) How should the surgical approach in thyroidectomy be selected? A prospective study comparing the trauma of 3 different thyroidectomy surgical approaches. Surg Laparosc Endosc Percutan Tech 30(1):22–25. https://doi.org/10.1097/SLE.0000000000000743ArticlePubMedPubMed CentralGoogle Scholar
- Lee J, Kwon IS, Bae EH et al (2013) Comparative analysis of oncological outcomes and quality of life after robotic versus conventional open thyroidectomy with modified radical neck dissection in patients with papillary thyroid carcinoma and lateral neck node metastases. J Clin Endocrinol Metab 98(7):2701–2708. https://doi.org/10.1210/jc.2013-1583ArticleCASPubMedGoogle Scholar
- Lee J, Nah KY, Kim RM et al (2010) Differences in postoperative outcomes, function, and cosmesis: open versus robotic thyroidectomy. Surg Endosc 24(12):3186–3194. https://doi.org/10.1007/s00464-010-1113-zArticlePubMedGoogle Scholar
- Tae K, Kim KY, Yun BR et al (2012) Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc 26(7):1871–1877. https://doi.org/10.1007/s00464-011-2116-0ArticlePubMedGoogle Scholar
- Kim WW, Jung JH, Lee J et al (2016) Comparison of the quality of life for thyroid cancer survivors who had open versus robotic thyroidectomy. J Laparoendosc Adv Surg Tech A 26(8):618–624. https://doi.org/10.1089/lap.2015.0546ArticlePubMedGoogle Scholar
- Bellotti C, Capponi MG, Cinquepalmi M et al (2018) MIVAT: the last 2 years experience, tips and techniques after more than 10 years. Surg Endosc 32(5):2340–2344. https://doi.org/10.1007/s00464-017-5929-7ArticleCASPubMedGoogle Scholar
- Costa B, Rodrigues DSB, Magalhaes DDD et al (2020) Quantitative ultrasound assessment of hyoid bone displacement during swallowing following thyroidectomy. Dysphagia. https://doi.org/10.1007/s00455-020-10180-5 (Epub ahead of print 2020/09/06) ArticlePubMedGoogle Scholar
- Im I, Jun JP, Crary MA et al (2019) Longitudinal kinematic evaluation of pharyngeal swallowing impairment in thyroidectomy patients. Dysphagia 34(2):161–169. https://doi.org/10.1007/s00455-018-9949-9ArticlePubMedGoogle Scholar
- Hyun K, Byon W, Park HJ et al (2014) Comparison of swallowing disorder following gasless transaxillary endoscopic thyroidectomy versus conventional open thyroidectomy. Surg Endosc 28(6):1914–1920. https://doi.org/10.1007/s00464-013-3413-6ArticlePubMedGoogle Scholar
- Jung SP, Kim SH, Bae SY et al (2013) A new subfascial approach in open thyroidectomy: efficacy for postoperative voice, sensory, and swallowing symptoms. A randomized controlled study. Ann Surg Oncol 20(12):3869–3876. https://doi.org/10.1245/s10434-013-3163-7ArticlePubMedGoogle Scholar
- Sinclair CF, Bumpous JM, Haugen BR et al (2016) Laryngeal examination in thyroid and parathyroid surgery: an American Head and Neck Society consensus statement. Head Neck 38(6):811–819. https://doi.org/10.1002/hed.24409ArticlePubMedGoogle Scholar
- Chun BJ, Bae JS, Lee SH et al (2015) A prospective randomized controlled trial of the laryngeal mask airway versus the endotracheal intubation in the thyroid surgery: evaluation of postoperative voice, and laryngopharyngeal symptom. World J Surg 39(7):1713–1720. https://doi.org/10.1007/s00268-015-2995-7ArticlePubMedGoogle Scholar
- Ryu JH, Han SS, Do SH et al (2013) Effect of adjusted cuff pressure of endotracheal tube during thyroidectomy on postoperative airway complications: prospective, randomized, and controlled trial. World J Surg 37(4):786–791. https://doi.org/10.1007/s00268-013-1908-xArticlePubMedGoogle Scholar
- Koo CH, Sohn HM, Choi ES et al (2019) The effect of adjustment of endotracheal tube cuff pressure during scarless remote access endoscopic and robotic thyroidectomy on Laryngo-Pharyngeal complications: prospective randomized and controlled trial. J Clin Med. https://doi.org/10.3390/jcm8111787ArticlePubMedPubMed CentralGoogle Scholar
- Xu YJ, Wang SL, Ren Y et al (2012) A smaller endotracheal tube combined with intravenous lidocaine decreases post-operative sore throat - a randomized controlled trial. Acta Anaesthesiol Scand 56(10):1314–1320. https://doi.org/10.1111/j.1399-6576.2012.02768.xArticleCASPubMedGoogle Scholar
- Exarchos ST, Lachanas VA, Tsiouvaka S et al (2016) The impact of perioperative dexamethasone on swallowing impairment score after thyroidectomy: a retrospective study of 118 total thyroidectomies. Clin Otolaryngol 41(5):615–618. https://doi.org/10.1111/coa.12547ArticleCASPubMedGoogle Scholar
- Aidan P, Pickburn H, Monpeyssen H et al (2013) Indications for the gasless transaxillary robotic approach to thyroid surgery: experience of forty-seven procedures at the American hospital of paris. Eur Thyroid J 2(2):102–109. https://doi.org/10.1159/000350854ArticlePubMedPubMed CentralGoogle Scholar
- Elzahaby IA, Fathi A, Abdelwahab K et al (2018) Endoscopic thyroidectomy using the unilateral axillo-breast approach versus the modified anterior chest wall approach: a prospective comparative study. Surg Laparosc Endosc Percutan Tech 28(6):366–370. https://doi.org/10.1097/SLE.0000000000000582ArticlePubMedGoogle Scholar
- Goswami S, Peipert BJ, Mongelli MN et al (2019) Clinical factors associated with worse quality-of-life scores in United States thyroid cancer survivors. Surgery 166(1):69–74. https://doi.org/10.1016/j.surg.2019.01.034ArticlePubMedGoogle Scholar
- Hashemian M, Khorasani B, Tarameshlu M et al (2019) Effects of dysphagia therapy on swallowing dysfunction after total thyroidectomy. Iran J Otorhinolaryngol 31(107):329–334. https://doi.org/10.22038/ijorl.2019.36233.2193ArticlePubMedPubMed CentralGoogle Scholar
- Kasperbauer JL (2004) Locally advanced thyroid carcinoma. Ann Otol Rhinol Laryngol 113(9):749–753. https://doi.org/10.1177/000348940411300914ArticlePubMedGoogle Scholar
- Nouraei SAR, Allen J, Kaddour H et al (2017) Vocal palsy increases the risk of lower respiratory tract infection in low-risk, low-morbidity patients undergoing thyroidectomy for benign disease: a big data analysis. Clin Otolaryngol 42(6):1259–1266. https://doi.org/10.1111/coa.12913ArticleCASPubMedGoogle Scholar
- Rosato L, Avenia N, Bernante P et al (2004) Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 28(3):271–276. https://doi.org/10.1007/s00268-003-6903-1ArticlePubMedGoogle Scholar
- Sasaki A, Nakajima J, Ikeda K et al (2008) Endoscopic thyroidectomy by the breast approach: a single institution’s 9-year experience. World J Surg 32(3):381–385. https://doi.org/10.1007/s00268-007-9375-xArticlePubMedGoogle Scholar
- Senise AT QD, Degani C, Correˆa LAC, Dedivitis RA, Lehn CN, Xavier C, Barros APB. (2009) Symptoms and signs of swallowing changes after thyroidectomy
- Wang C, Feng Z, Li J et al (2015) Endoscopic thyroidectomy via areola approach: summary of 1,250 cases in a single institution. Surg Endosc 29(1):192–201. https://doi.org/10.1007/s00464-014-3658-8ArticlePubMedGoogle Scholar
- Yoon JH, Park CH, Chung WY (2006) Gasless endoscopic thyroidectomy via an axillary approach: experience of 30 cases. Surg Laparosc Endosc Percutan Tech 16(4):226–231. https://doi.org/10.1097/00129689-200608000-00006ArticlePubMedGoogle Scholar
- Yu ST, Chen WZ, Xu DB et al (2019) Minimally invasive video-assisted surgical management for parapharyngeal metastases from papillary thyroid carcinoma: a case series report. Front Oncol 9:1226. https://doi.org/10.3389/fonc.2019.01226ArticlePubMedPubMed CentralGoogle Scholar
- Zhang Z (2014) Efficacy comparison of the anterior low small incision and the traditional incision for treatment of thyroid adenoma. Pak J Med Sci 30(5):1119–1122. https://doi.org/10.12669/pjms.305.4767ArticleCASPubMedPubMed CentralGoogle Scholar
Funding
The authors did not receive any funding or support for the submitted work.